Telehealth visits rose markedly in response to the pandemic, with patients turning to health care by phone or video for their routine checkups, dermatology, and eye exams as well as screening for COVID-19. By increasing telehealth, California may be able to expand health care access for rural residents, persons with disabilities, and low-income individuals—who may lack transportation or the flexibility to leave work for appointments. Although underserved groups stand to gain from more telehealth, in the past they have lagged in taking up virtual health care.
One reason may be a lack of access to fast internet—both rural and low-income Californians are less likely to have broadband, though a $7 billion federal investment in connectivity along with earlier relief funds could transform the broadband infrastructure landscape. Language barriers are another concern. Patients with limited English proficiency were already less likely to use telehealth in California, and the need for appropriate language services is pressing. The pandemic also brought competing demands on bandwidth and devices as household members work from home, attend school, or meet other daily needs online.
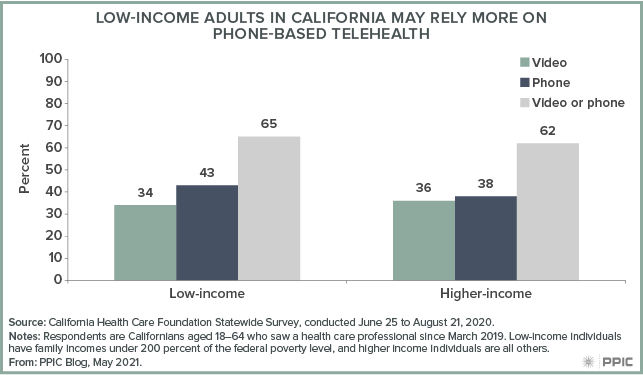
Yet telehealth has expanded, even for hard-to-reach groups. A group of community clinics, which serve many low-income patients in California, went from conducting less than 1% of their patient encounters through telehealth in February 2020 to around half of encounters just a few months later. Low-income patients are more likely to have telehealth visits by phone rather than video compared to higher-income Californians. And it is promising that they are satisfied with the telehealth experiences they have, and want to continue using the tool.
Furthermore, telehealth has become a vital tool for delivering behavioral health, including individual or group therapy. For many, the pandemic brought isolation, coronavirus-related worries, and financial difficulties even as it reduced access to familiar supports and routines. The consequences include poor mental health and surging drug overdoses. Low-income Californians were more likely to report worse mental health since the start of the pandemic, suggesting high need for behavioral health services.
Both private health insurance companies and public programs like Medi-Cal and Medicare have demonstrated flexibility in reimbursing telehealth visits, easing worries over what is covered while allowing out-of-state providers to treat patients in California. Such flexibility helped augment a strained supply of behavioral health services that pre-dated the current crisis. However, changes to licensing requirements will be needed to continue some of these relationships.
The state’s plans for after the pandemic signal an ongoing commitment to telehealth and its role for underserved groups. The Department of Health Care Services, which runs Medi-Cal, has proposed extending many temporary telehealth changes, including some phone-based care important to low-income patients. Telehealth’s promise in California is most likely to be realized through policies like these that prioritize health equity along with expansion.



