This post is part of a series reflecting on California’s experience of the COVID-19 pandemic.
The rapid spread of COVID-19 two years ago led California to declare a public health emergency, a state of emergency that remains in effect through this March. The heaviest burdens of the pandemic—death, illness, and economic hardship—fell disproportionately on Californians who are low-income, Black, Latino, or frontline workers. The pandemic not only highlighted entrenched health disparities among some groups but it also underscored how critical insurance coverage and access to health care are for all Californians.
The COVID-19 death rate
Nearly 84,000 Californians have died from COVID-19 since the pandemic began—about 212 deaths per 100,000 residents, according to state data. Older Californians died at far higher rates than younger adults, with about 985 deaths per 100,000 seniors 65 and older, compared to about 102 deaths per 100,000 for adults under 65.
Disparities were also stark across race and ethnicity. Black residents died at a rate 37% higher than white residents; for Latino residents, death rates were 20% higher.
The higher death toll among Latinos is particularly troubling given their younger age profile compared to whites. Latinos account for 44% of COVID-related deaths but only about 36% of California residents over 18—and this masks larger disparities for certain age groups, including some younger Latinos. For example, nearly two-thirds of COVID-related deaths among adults under 50 are Latinos, who comprise less than half of the state’s population in that age group.
COVID vaccination
Less than a year ago, in May 2021, Californians over 12 became eligible for a free COVID vaccine—older Californians and those with certain health conditions were eligible earlier. California has since made good progress on vaccinating residents; about 83% of eligible Californians (ages 5 and older) had received at least one vaccine dose as of March 1, 2022, though only about 57% of those eligible had received a booster shot.
Vaccination rates do vary across California’s diverse regions and communities. Smaller counties in the north have some of the lowest overall rates—in some places fewer than 50% of the population has been vaccinated. Counties in the San Joaquin Valley and other inland areas have lower vaccination rates than the Bay Area and coastal counties.
Medi-Cal’s role in the pandemic
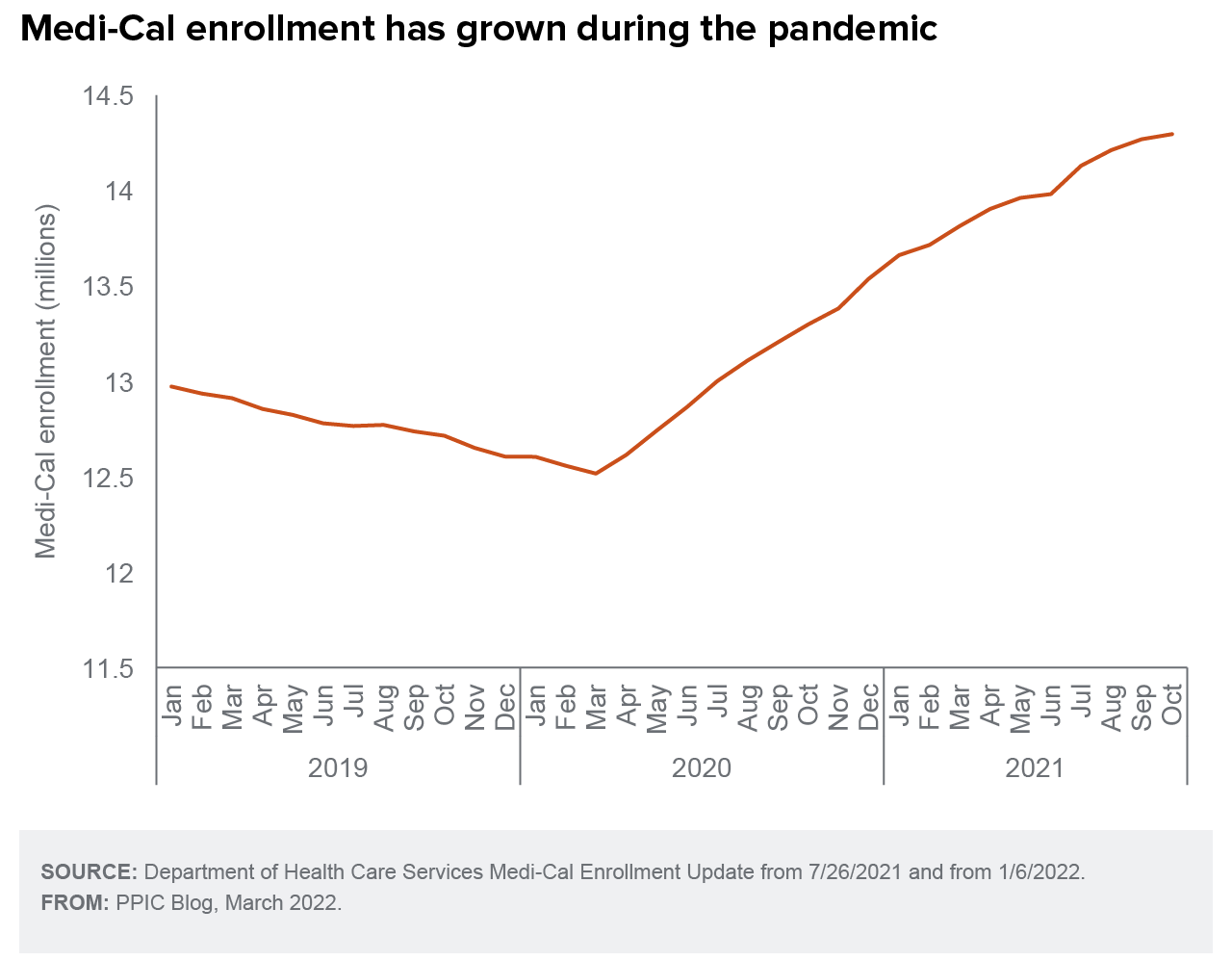
Medi-Cal now covers over one-third of the state’s residents. In October 2021, 14.3 million low-income residents were enrolled. Program enrollment has been growing while the state pauses periodic eligibility checks due to COVID-19, a move that the federal government required of states in exchange for increased funds during the public health emergency.
There is also new flexibility around reimbursement during the pandemic, wherein patients can switch to telehealth if in-person visits feel like a risk. And Medi-Cal covers COVID-19 treatment for all low-income Californians who fall ill, regardless of immigration status. Currently, COVID vaccination rates among those covered by Medi-Cal are more than 25 percentage points lower than all Californians.
Changes in the health care workforce
After layoffs early in the pandemic and workers departing as the crisis persisted, health care now faces a staffing shortage. Nurses exhausted by COVID-19 have been leaving their jobs, resulting in a nursing shortage in California hospitals.
The profession is also losing some of its most experienced workers. Many older registered nurses retired in 2020, or reported plans to retire or leave nursing in the following two years, exacerbating a scarcity.
Looking ahead
California’s public health emergency could end at the end of March while the federal declaration could end mid-April. Medi-Cal will then resume reviews of eligibility, and many Californians could lose coverage if their income or family circumstance have changed or they fail to complete the required forms. The state will also lose increased federal Medi-Cal funding received throughout the pandemic.
Even as pandemic policies disappear, projects stalled by the pandemic are returning—the Healthy California for All Commission is again analyzing how the state can provide affordable health coverage to all state residents. Insights from the upcoming report from the commission will be valuable to providing Californians access to the medical care they need.





